Strength
Skeletal muscle weakness is present in patients with chronic respiratory conditions and this weakness can affect lower limb strength.
Strength training can improve muscle strength, peak work capacity and endurance time.
A combination of strength and endurance training results in greater increases in both strength and endurance than either form of training alone.
Strengthening the muscles in the lower limbs is important as these muscles are used everyday. A relationship has been shown between lower limb strength and lower limb work capacity. Having stronger lower limb muscles may help patients to perform short bursts of activity (such as getting on a bus), and may also reduce falls.
Strengthening the muscles in the upper limbs is also important as these muscles are used everyday. Studies indicate that strength training for the upper limb muscles results in moderate improvements in upper limb strength.20A relationship has been shown between upper limb strength and upper limb work capacity for patients with COPD which suggests that having stronger upper limb muscles may help patients perform functional tasks (i.e. by enhancing the strength of the biceps and triceps muscles).
The studies that have examined strength training for the upper limbs have focused on the accessory muscles of inspiration and muscle groups used in everyday functional tasks. These muscles include:
- Pectoral muscles
- Latissimus dorsi
- Trapezius
- Biceps
- Triceps
Upper limb strength training can be combined with upper limb endurance training in a comprehensive program in order to gain the benefits from both modes of training.21
Skeletal muscle dysfunction is also common in ILD (1). In addition, reductions in muscle force correlate with the level of lung impairment and reduced peak exercise capacity (2,3). Therefore, improving muscle strength and function should also be an important goal of PR for patients with ILD.
- Panagiotou, M., V. Polychronopoulos, and C. Strange, Respiratory and lower limb muscle function in interstitial lung disease. Chronic Respiratory Disease, 2016. 13(2): p. 162-172.
- Nishiyama O, Taniguchi H, Kondoh Y, Kimura T, Ogawa T, Watanabe F, Arizono S. Quadriceps weakness is related to exercise capacity in idiopathic pulmonary fibrosis. Chest. 2005; 127( 6): 2028– 33.
- Watanabe F, Taniguchi H, Sakamoto K, Kondoh Y, Kimura T, Kataoka K, Ogawa T, Arizono S, Nishiyama O, Hasegawa Y. Quadriceps weakness contributes to exercise capacity in nonspecific interstitial pneumonia. Respir Med. 2013; 107( 4): 622– 8.
An adequate strengthening program can be devised with or without portable (e.g. free weights or elastic bands) or fixed weight equipment and a person’s own body weight may be sufficient stimulus. Exercises should be performed slowly and smoothly.
It is generally recommended to perform the arm exercises in the in the sitting position with back supported. However, in everyday life upper limb activities are often carried out in standing. Some of the exercises can be performed in standing providing the patient can perform a correct technique.
Examples of lower limb strengthening exercises without weight machines are listed below
Lower Limb Strength Exercises
(high weight and low repetition)
| Exercise #1 Knee extensions in sitting |
 |
|
| Exercise #2 Squats |
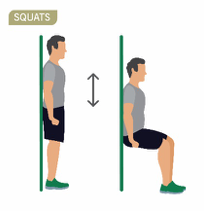 |
|
| Exercise #3 Climbing stairs or use a stepping box |
 |
|
Tip: It is often advisable to perform lower limb endurance training as a “warm-up” before strength training.
Examples of upper limb strengthening exercises without weight machines are listed below. The program Exercise Professional needs to review the most appropriate exercises based on the patient’s active range of motion (ROM) and consider any past or present shoulder/upper limb musculoskeletal concerns.
Upper Limb Strength Exercises
(high weight and low repetition)
| Shoulder press |  |
The following exercises were adopted from: Lung Foundation Australia’s Better Living with Exercise- Your Personal Guide
|
| Bicep curl | 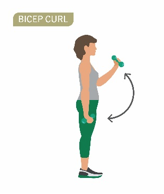 |
|
| Wall press | 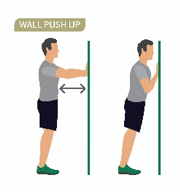 |
|
Strength training with fixed weight machines:
Lower limb:
- Leg press.
- Quadriceps extension.
Upper limb:
- Lat/chest pull down for latissimus dorsi.
- Chest press for pectorals.
- Upright cable pull for trapezius
For patients with lung cancer after surgery, upper limb weights should be used with caution due to wound healing. Patients usually require 6 to 8 weeks postoperative for healing to occur prior to commencement of resistance exercises (recommend medical clearance before commencement).
The appropriate intensity for strengthening exercises can be prescribed based on:
A. One repetition maximum.
B. Weight repetitions.
A. Prescribing intensity based on one repetition maximum
The maximum weight that can be lifted once by a particular muscle group is known as the one repetition max (1 RM)*. The 1 RM value is used to prescribe the intensity of the strength training program:
How to perform a 1 repetition maximum 1 RM
- Warm up by completing several submaximal contractions (e.g. leg press 5kg)
- Determine the 1 RM within four trials with rest periods of 3-5 minutes between trials
- Select an initial weight that is within the person’s perceived capacity (50-70% of capacity)
- Progressively increase the resistance by 2.5-20kg until they cannot complete the repetition
- Record the final weight lifted successfully as the absolute 1 RM
Example:
Leg press – warm up 5kg
1 repetition of 10kg = success -> rest
1 repetition of 15kg = success -> rest
1 repetition of 20kg = success -> rest
1 repetition of 25kg = failure -> 1 RM = 20kg
Choose an exercise with a weight that can be performed 8-12 times with correct technique.
- Start with a weight of 60 to 80% of the patient’s 1 RM weight.
- Perform one set (8-12 repetitions) of a particular exercise.
- Aim to increase the weight up to 80% of the patient’s 1 RM while ensuring that the patient performs the exercise with the correct technique.
- After the patient can perform three sets of an exercise, the weight may be increased.
*Caution: Testing pulmonary rehabilitation patients for their 1 RM may not be advisable. There may be concerns regarding joints, ligaments and bone density in many of these patients.
B. Prescribing intensity based on weight repetitions
To avoid problems with testing patients for their 1 RM, the intensity of exercise may be prescribed in either of the following ways:
- Use a sub-maximal test to estimate the patient’s 1 RM. The patient lifts a weight that they can only lift 2 to 3 times; this weight is taken as 80% of the patient’s 1 RM. From this, the 1 RM can be calculated and the intensity prescribed as for the 1 RM method (see above).
- Complete a 10RM test by following the same steps to performing a 1 RM test but working with 10 repetitions at a time and using this weight as the starting weight.
For patients with lung cancer after surgery, upper limb weights should be used with caution due to wound healing. Patients usually require 6 to 8 weeks postoperative for healing to occur prior to commencement of resistance exercises (recommend medical clearance before commencement).
- Perform one set (8-12 repetitions) of a particular exercise, then rest for 2-3 minutes.
- Once the patient can perform 2-4 sets of a particular exercise, the weight can be increased by 5% or between 0.5 kg to 5 kg depending on which muscle group is being trained (smaller increments for smaller muscle groups and larger increments for larger muscle groups). For upper body strength training, ask the patient to move their arms up as they breathe in, and down as they breathe out.
- Some exercises can be performed in the sitting position, with the back supported where possible.
- These exercises should not cause significant discomfort to joints.
The duration of a strength training session will be the time it takes to complete the appropriate number of sets.
The frequency for strength exercise sessions should be two or three times per week. Patients should ensure they have at least one day of rest between strength training sessions.


