Breathe Easy Walk Easy Lungs for Life (BE WELL)
A National Health and Medical Research Council (NHMRC) Global Alliance for Chronic Diseases (GACD) funded project.
Nine resources have been developed to assist Aboriginal and Torres Strait Islander Health Workers and Practitioners yarn about Chronic Obstructive Pulmonary Disease (COPD) with Aboriginal and/or Torres Strait Islander peoples living with COPD.
Aboriginal and/or Torres Strait Islander Health Workers and Practitioners may work together with doctors, physiotherapists, exercise physiologists, nurses, psychologists, dietitians and other health professionals to provide high quality care.
The resources on this webpage were developed as part of a National Health and Medical Research Council funded study that partnered with Aboriginal Community Controlled Health Services (ACCHS) to trial the implementation of pulmonary rehabilitation. These resources form the basis of the education component of a pulmonary rehabilitation program.
These resources are to guide Aboriginal health workers in yarning about each topic. The language can be changed to suit the local community. Using examples and analogies relevant to each community is encouraged to support understanding.
TOPIC 1: HOW THE LUNGS WORK
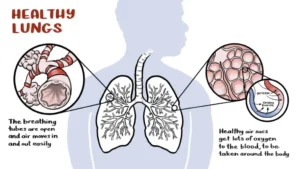
Healthy Lungs – Yarning illustration 1
There are 2 lungs (left and right) that sit inside the ribs. The purpose of the lungs is to get fresh air (oxygen – “good air”) into the body and remove old air (carbon dioxide – “bad air”).
When breathing in, the air enters the lungs through the nose and mouth and travels down the windpipe (trachea). Next it goes through the airways (bronchi) to the air sacs (alveoli).
When the (oxygen) reaches the air sacs (alveoli) it meets with small blood vessels (capillaries). Here, the oxygen moves into the blood and is taken around the body to where it is needed. The old air (carbon dioxide) moves out of the blood into the air sacs and is breathed out.
TOPIC 2: WHAT HAPPENS IN THE LUNGS IN COPD
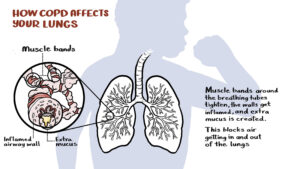
What happens in the lungs in COPD – Yarning illustration 2a
If someone has COPD, the lungs change:
A) The airways narrow (Yarning illustration 2a).This is because:
- the walls of the airways become inflamed (swollen),
- the small muscle bands around the airways tighten and
- more mucus/spit is produced and partly fills the airways.
Narrow airways means less air flows in and out of the lungs.
These changes are sometimes called chronic bronchitis
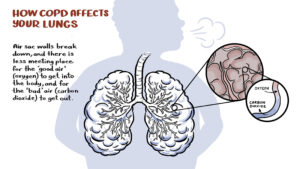
What happens in the lungs in COPD – Yarning illustration 2b
B) The air sacs are damaged (Yarning illustration 2b) and there are less ‘meeting places’ where oxygen moves into the blood and carbon dioxide moves out. This damage to the air sacs is called emphysema.
Health Professional Note: for additional resources to understand symptoms and management of COPD, including chronic bronchitis and emphysema, access COPD page on the LFA website.
TOPIC 3: MEDICATIONS, HOW TO USE INHALERS, ACTION PLANS
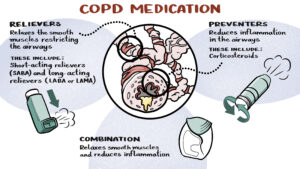
Medications and how to use inhalers – Yarning illustration 3a
Some medications help open the airways (i.e. make them less narrow) and let more air move in and out of the lungs (Yarning illustration 3a).
These medications are:
- Relievers that relax the small muscles around the airways.
- Note for health professionals: for example, Ventolin is a short acting beta agonist (SABA) or Onbrez Breezhaler which is a long-acting beta agonist (LABA) or Spiriva which is a long-acting muscarinic antagonist (LAMA).
- Preventers reduce the inflammation of the airway walls.
- Note for health professionals: for example inhaled corticosteroids (ICS) such as Fluticasone.
- Sometimes these reliever and preventer medications are put together in in a combination therapy inhaler (for example, Seretide).
Health professional resource:
- Chart of Inhalers for COPD provides the names of most of the inhaled medications currently prescribed.
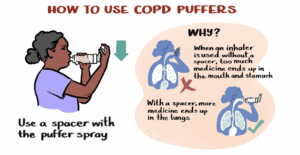
Learning how to take inhalers – Yarning illustration 3b
Taking inhaled medications correctly is very important for managing COPD.
Inhaler medications come in lots of different types of devices. Each device has different instructions for how to prepare, use and look after it.
If a person is using a ‘puffer spray’ then using a spacer will help to get the most medication into the lungs where it is needed.
Yarning illustration 3b shows that without a spacer most of the medication (little dots in the picture above) goes into the stomach. With the spacer most of the medication goes into the lungs where it is needed.
Health professional resource:
You may like to watch the relevant video/s with the person living with COPD to make sure they are using their inhalers correctly.
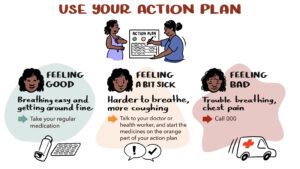
Action Plans – Yarning Illustration 4
It is very important for a person living with COPD to have a COPD Action Plan, so they know what to do if they start to feel sick.
In the action plan is like traffic lights:
- the Green section lists the medications that the person takes regularly
- the Orange section lists the medications that a person would take if they start to feel a bit sick, such as finding it harder to breathe, more coughing etc. They should also make an appointment to see their doctor.
- the Red section is when a person is feeling really sick, such as trouble breathing, chest pain. This is when they should call an ambulance – 000.
If the person does not have an Action Plan, organise an appointment with their doctor so they can develop an Action Plan together.
TOPIC 4: WHY EXERCISE IS IMPORTANT
Benefits of exercise training: endurance and strength training – Yarning illustrations 5a
What happens if a person doesn’t exercise (Yarning illustrations 5a- left hand side of the illustration)
When people do not exercise or are not physically active they get less fit and weaker.
When a person has COPD, they can become more breathless when they move, which means they are less active. This may mean they get less fit and when doing regular activities such as shopping, cleaning or looking after kids they feel even more breathless. This is called the spiral of inactivity (disability spiral) where the less someone does, the worse they may get and even small amounts of moving may make them breathless.
What changes when a person with COPD does fitness training (Yarning illustrations 5a- right hand side)
In a pulmonary rehabilitation program, fitness training like walking on a treadmill, walking on a flat track inside or outside, or riding a stationary cycle aims to reverse this spiral of inactivity (disability spiral) so that a person living with COPD can move more and feel less breathless.
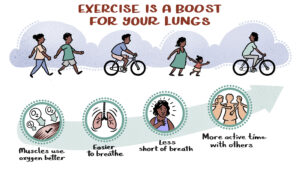
Benefits of fitness training – Yarning illustration 5b
This type of fitness training (walking on a treadmill, walking on a flat track inside or outside, or stationary cycling) helps the muscles use oxygen better, breathing improves, and the person will feel less breathless when being active.
This means someone with COPD can do more at home and with family, friends and community.
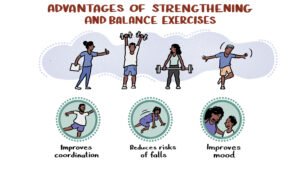
Strength and balance training – Yarning illustration 5c
In pulmonary rehabilitation, someone with COPD will also do exercises for their strength and balance, which can help to reduce the risk of falls and make them generally feel better.
TOPIC 5: MANAGING BREATHLESSNESS AND HOW TO CONSERVE ENERGY
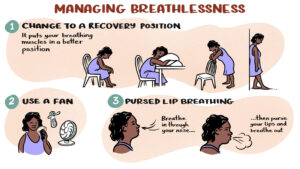
Managing breathlessness – Yarning Illustration 6
People with COPD often get breathless when being active or feeling unwell.
There are ways to help manage breathlessness. Using one of the recovery positions helps the breathing muscles to work better. Most of these positions are leaning forward and having the arms supported so the muscles around the neck and upper chest can work better to help breathing.
Using a battery driven hand-held fan can also help by cooling the face.
Pursed-lip breathing when in the recovery positions or when feeling breathless during activity can help reduce breathlessness. Pursed-lip breathing is where a person tightens (‘purse’) their lips, as if they were going to whistle when breathing out through the mouth.
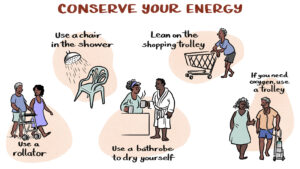
Energy conservation – Yarning illustration 7
Although it is very important to do fitness and strength training, sometimes people with COPD may need to conserve energy to manage regular activities.
Tips and tricks to help reduce breathlessness during regular activities:
- Using a walking aid (rollator) may help the person to get out and about.
- Sitting on a chair or stool while showering.
- Using a towelling bathrobe for drying after showering
- Leaning on a shopping trolly in the supermarket (this is an example of the recovery position with arms supported that we talked about under managing breathlessness).
- If using oxygen, pull it in a light-weight trolley instead of carrying it.
TOPIC 6: MANAGING ANXIETY AND STRESS
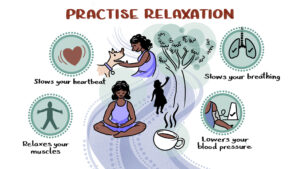
Relaxation – Yarning illustration 8
Many people with COPD get stressed or anxious, which can make them feel more breathless.
Learning relaxation techniques is important for managing stress and anxiety. These techniques help to relax the muscles, slow breathing, and lower heart rate and blood pressure.
This means the body is not working as hard and the person may feel calmer and less breathless. Encourage the person with COPD to find out what relaxation techniques work for them, for example sitting quietly outside and thinking about a pleasant calm picture in their mind, having a cup of tea, or talking to or patting their dog or cat.
The healthcare team (including a physiotherapist or exercise physiologist) can help people with COPD to learn these techniques. A person with diagnosed anxiety and/or depression, may be referred to a psychologist for more support.
Professional Note: It might be beneficial to have local/ regional mental health lines on hand that people can call for more support if necessary.
TOPIC 7: HEALTHY EATING, ESPECIALLY IF YOU ARE BREATHLESS AND TIRED
Healthy Eating – Yarning illustration 9
It is important that a person with COPD eats food that is healthy to keep them well. Some people with COPD find it hard to eat and prepare food because of breathlessness. Some ways to manage healthy eating when breathless, are:
- resting before meals,
- eating slowly, or pacing and breathing while chewing,
- having smaller and more frequent meals,
- having food provided or assistance with preparation of meals,
- preparing extra meals when feeling well,
- stocking up healthy and convenient meals.
The healthcare team (including a physiotherapist or exercise physiologist) can help with these strategies. In some cases, a person with COPD may be referred to a dietitian for support.
ACKNOWLEDGEMENTS:
These resources were developed with funding from the NHMRC Global Alliance for Chronic Diseases for a project tilted: Implementing evidence into practice to improve chronic lung disease management in Indigenous Australians: the Breathe Easy, Walk Easy – Lungs for Life (BE WELL) project.
The development of the resources was led by Professor Jennifer Alison and Dr David Meharg, with support from Lung Foundation Australia.
The scripts were reviewed by Aboriginal and Torres Strait Islander health professionals.
The Investigation team for the NHMRC GACD grant was: Prof Jennifer Alison, Prof Christine Jenkins, Prof Stephen Jan, Prof Graeme Maguire, Prof Tim Shaw, Prof Sarah Dennis, A/Prof Zoe McKeough, Dr Vanessa Lee.
Related publications:
1. Meharg DP, Dennis SM, McNab J, Gwynne KG, Jenkins CR, Maguire GP, Jan S, Shaw T, McKeough Z, Rambaldini B, Lee V, McCowen D, Newman J, Monaghan S, Longbottom H, Eades SJ, Alison JA (2023). A mixed methods study of Aboriginal health workers’ and exercise physiologists’ experiences of co-designing chronic lung disease ‘yarning’ education resources. BMC Public Health 23(1): 612. DOI: 10.1186/s12889-023-15508-y
2. Meharg DP, Dennis SM, McNab J, Gwynne KG, Jenkins CR, Maguire GP, Jan S, Shaw T, McKeough Z, Rambaldini B, Lee V, McCowen D, Newman J, Monaghan S, Longbottom H, Eades SJ, Alison JA. A qualitative study of Aboriginal peoples’ health care experiences with chronic obstructive pulmonary disease. Qualitative Health Research. 2025 Feb;35(2):216-233: https://doi.org/10.1177/10497323241259891